A new approach to treating coronary artery disease.
Our Company

We’re on a mission to prevent heart attacks.
At Abcentra, we are a clinical-stage biopharmaceutical company focused on bringing new and better treatment options to patients with coronary artery disease, with the aim of preventing heart attacks.
Our team is pioneering the concept of oxidized low-density lipoprotein (OxLDL) inhibition – a selective way to target coronary artery inflammation. OxLDL inhibition has promise to target coronary inflammation in a highly specific manner, thereby maximizing the potential benefit to patients and minimizing treatment-associated risks.
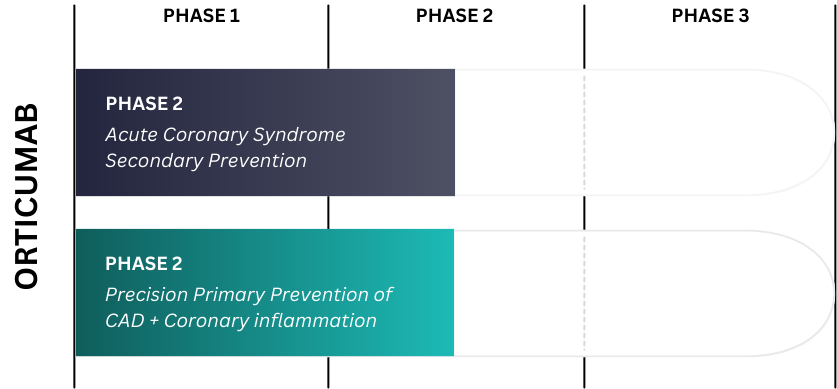
Our clinical-stage product, Orticumab, is a first-in-class oxLDL inhibitor antibody therapy that has now demonstrated the potential to reduce coronary inflammation in a phase 2a study. We are developing Orticumab for secondary prevention after an acute coronary syndrome (ACS), with further plans to expand use into coronary artery disease patients with elevated coronary inflammation.
Our Leadership Team
Meet the leading scientists, business leaders, and passionate advocates leading Abcentra’s executive team and Board of Directors.

Our mission to combat arterial inflammation isn’t just about developing a drug, it is about rewriting the narrative around cardiovascular health. We believe in a future where the message of every heartbeat is vitality – not vulnerability.
Chris Farina – CEO, Abcentra
Our Advisors & Investors
Our success is the culmination of many partnerships, relationships, and investments. Meet some of our most important advisors and investors.